Liberia: Filling the Health Care Workforce Gaps (2012-Current)
Highlights
- Assessing barriers to retention in HIV care in Monrovia, Liberia. Grant funded by UMB Center for Global Education Initiatives for interprofessional students to explore the context of care, barriers to HIV/other care, and the impact of the social determinants on HIV care and treatment in a developing country in West Africa. Students compared and contrasted the similarities/differences between Monrovia, Liberia and Baltimore, Maryland as it relates to HIV care, treatment, and support (2017).
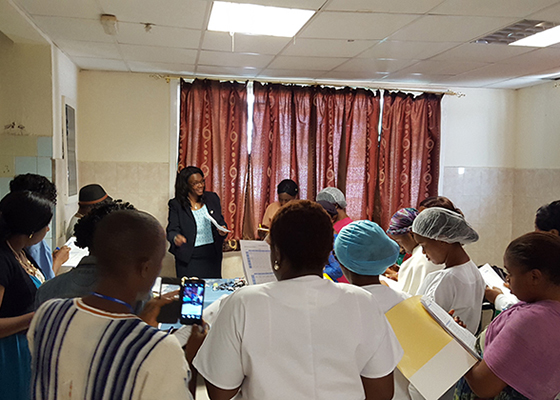
- Post Ebola Health System Strengthening - Neonatal Nurse Training Program (photos). Catholic Relief Services. Development and Implementation of a post-graduate training module for neonatal nurses in collaboration with Catholic Relief Services and Mother Patern College of Health Sciences, Monrovia, Liberia (2016).
- Presentations prepared for UMB Ebola Symposium: "Ebola: Who is Under the Personal Protective Equipment in Liberia" and "The Impact on Nursing Workforce Locally and Globally" (2014).
Background
The 14-year civil crisis in Liberia lead to the destruction of hospitals and clinics and the shutdown of most educational programs, causing medical professionals to leave the country and a devastated economy. With a life expectancy of 63 years of age and an infant mortality rate of 24th in the world, Liberia is struggling to address the basic health needs of its current population. Registered nurses (RNs), midwives, and physician assistants (PAs) account for 70 percent of the health care workforce and are the backbone of the health sector often working in rural, underserved communities, with a scarcity of physicians. Within these settings, nurses and PAs routinely engage in clinical and public health leadership responsibilities above and beyond their training and education in order to address the high burden of disease presenting at all levels of the health care system.
During the Ebola Virus Disease (EVD) outbreak of 2014, nurses/midwives and non-professional healthcare workers proved to be loyal and committed to the communities that they serve. Despite valiant efforts that saved lives, gaps in nursing capacity and suboptimal competencies became increasingly visible. To build a strong healthcare system that is ready, motivated, and competent to deal with current and unanticipated health challenges, nursing and other health professionals’ capacity and competency must be optimized. By doing so, Liberia can increase its capacity to respond and adapt to planned and unplanned needs, and absorb shocks, such as a disease outbreak, natural disaster, or conflict.
Collaborative Goals
The Office of Global Health, in collaboration with the Mother Patern College of Health Sciences (MPCHS) in Liberia, have adapted and propose to implement a Primary Health Care Clinical Specialist (PHC-CS) master's program to increase the competence of workers and quality of patient care. The initial needs assessment was implemented by UMSON in May-June 2012 through key interviews, curricula reviews, and site visits. The outcome was a customized PHC-CS program framework for the Liberian healthcare context that would offer effective recruitment and workforce retention strategy. The ultimate aim of the master’s program is to reduce child and maternal mortality, improve maternal health, and battle major diseases ravaging the country.
